📞Customer Service: +86 13248368268 📧servicecenter@suzhoufrank.com one year replacement and warranty!
Master Bronchoscopy Anatomy & Techniques
Master bronchoscopy anatomy and techniques for improved patient care. Explore anatomy, skill enhancement, and technology innovations in this essential guide.
Dr Qi Rui
11/25/20253 min read
By Dr. Qi Rui, MD, FCCP – Consultant Pulmonologist & Interventional Bronchoscopy Trainer
Reviewed by: Prof. Alan Stewart, PhD – Medical Simulation Researcher & Developer of Clinical Training Systems
Summary
Bronchoscopy remains a cornerstone in respiratory diagnostics and therapeutic interventions. Mastery of bronchoscopy anatomy, refined navigation of the airway using bronchial anatomy bronchoscopy knowledge, and continuous bronchoscopy skills improvement are essential for safe, high-quality clinical performance. As technology evolves, the bronchoscopy simulator has emerged as a key driver of competency-based training, offering risk-free, realistic, and standardized skill development. This article outlines the anatomy, the techniques, the clinical applications, and the future directions shaping modern bronchoscopy practice.
Full Article
The Foundations of Bronchoscopy
Bronchoscopy is a minimally invasive procedure used to visualize the trachea, bronchi, and distal airways with either flexible or rigid bronchoscopes. Flexible scopes remain the gold standard for routine evaluations due to their versatility and patient comfort, while rigid scopes maintain value in emergency airway management, foreign body extraction, and complex therapeutic interventions.
Bronchoscopy plays a central role in:
Diagnosis of lung infections, tumors, and airway abnormalities
Biopsy and cytology sampling
Removal of secretions, obstructions, or foreign material
Interventional procedures in COPD, stenosis, and bleeding management
High-quality outcomes rely on a clinician’s familiarity with device mechanics, airway mapping, and procedural planning.
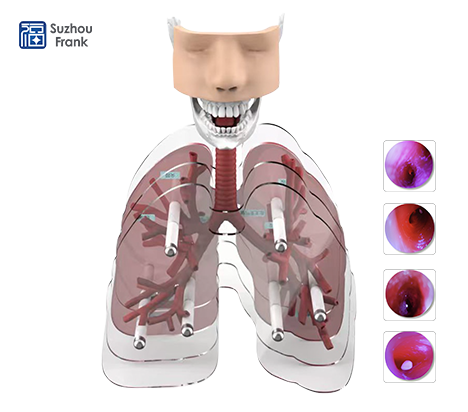
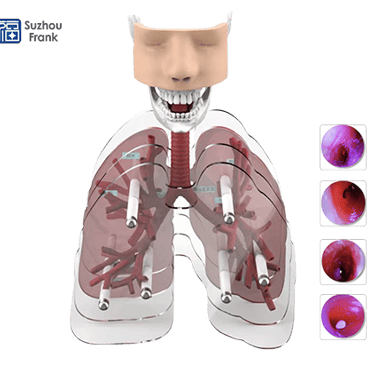
Bronchoscopy Anatomy and Airway Navigation
Successful bronchoscopy begins with a precise understanding of bronchoscopy anatomy. The bronchial tree provides the structural roadmap that guides safe navigation:
Key components of bronchial anatomy bronchoscopy
Trachea: The entry conduit; its cartilaginous rings offer tactile orientation.
Carina: A critical bifurcation landmark dividing the airway into right and left main bronchi.
Right Main Bronchus: Shorter, wider, and more vertical—more prone to foreign body entry.
Left Main Bronchus: Longer and more oblique, requiring controlled angulation.
Lobar and Segmental Bronchi: Essential for targeted inspection, lavage, and biopsy.
Clinicians trained in the nuances of bronchial branching patterns reduce procedural risks such as mucosal trauma, bleeding, or misplacement. Anatomical variations—stenosis, anatomical deformation, or postsurgical changes—must also be recognized and accommodated during bronchoscopy.
Tools, Techniques, and Clinical Application
Two primary types of bronchoscopes define modern practice:
Flexible Bronchoscopy
Preferred for diagnostics and routine therapeutics
Provides excellent maneuverability
Minimizes patient discomfort
Supports lavage, brushings, biopsy, and navigation to peripheral lesions
Rigid Bronchoscopy
Superior for airway foreign bodies
Facilitates large biopsy samples
Allows extensive therapeutic maneuvers
Critical in emergency airway control
Matching the instrument to the clinical scenario enhances safety and procedural efficiency.
Bronchoscopy Skills Improvement: Pathway to Competency
In today’s competency-based medical landscape, bronchoscopy skills improvement requires continuous, structured training rather than sporadic exposure.
Key strategies include:
Hands-on workshops & skill labs
Mentorship and supervised clinical practice
Post-procedure review and performance audits
Case-based learning for complex scenarios
Consistent, deliberate practice drives mastery, confidence, and clinical accuracy.
The Rising Importance of the Bronchoscopy Simulator
A bronchoscopy simulator is now considered essential to modern respiratory training programs. Simulation-based learning offers:
Zero-risk practice for beginners
Standardized exposure to rare and high-risk cases
Realistic airway resistance and visual feedback
Performance metrics for structured assessment
Enhanced preparedness for emergencies
Simulation accelerates learning curves, reduces patient risk, and supports lifelong professional development.
Safety, Complications, and Patient-Centered Care
Although bronchoscopy is generally safe, complications such as hypoxia, bleeding, infection, or pneumothorax can occur. Robust pre-procedure evaluation, sedation management, and vigilant monitoring mitigate these risks.
Best practices in patient care include:
Clear communication of risks and benefits
Obtaining informed consent
Monitoring during and after bronchoscopy
Providing clear post-procedure instructions
High-quality patient care builds trust and ensures safe recovery.
Future Directions: Technology Reshaping Bronchoscopy
Bronchoscopy is rapidly evolving, driven by innovation in digital imaging, simulation, and artificial intelligence. Expect significant advancements in:
AI-driven lesion recognition and navigation support
Augmented Reality (AR) overlays for training and live procedures
High-resolution real-time imaging with enhanced depth perception
Next-generation simulators replicating fluid dynamics, pathology variations, and emergency scenarios
These technologies promise higher precision, earlier diagnosis, and safer interventions.
Conclusion
Bronchoscopy is an indispensable tool in modern respiratory medicine. Mastery requires deep understanding of bronchoscopy anatomy, precise interpretation of bronchial anatomy bronchoscopy, deliberate bronchoscopy skills improvement, and the integration of advanced technologies such as the bronchoscopy simulator. As innovations continue to reshape the clinical landscape, clinicians who invest in continual learning will deliver superior patient outcomes and remain at the forefront of interventional pulmonology.
© 2025. All rights reserved.
About Us
Introduction
Development
Cooperation
Service
Main Products
Medical Grade Monitor
No 15, Jinyang road KunshanSuzhou, Jiangsu, China