📞Customer Service: +86 13248368268 📧servicecenter@suzhoufrank.com one year replacement and warranty!
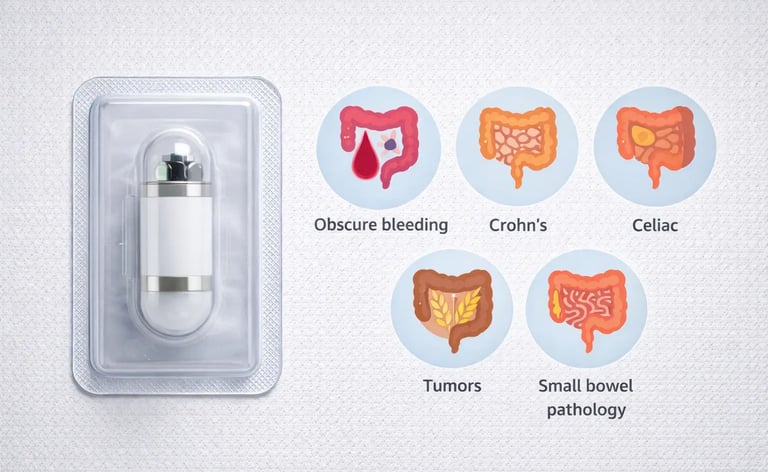
What Conditions Can Capsule Endoscopy Diagnose?
Capsule endoscopy diagnoses conditions standard scopes can't reach. Covers obscure bleeding , Crohn's , celiac , tumors and other small bowel pathology.
ENDOSCOPY
Dr Qi Rui
12/23/20256 min read
Capsule endoscopy opened a window into the small intestine that traditional scopes couldn't reach. For decades , the roughly 20 feet of small bowel between the stomach and colon remained largely inaccessible to direct visualization. Standard upper endoscopy reaches the duodenum. Colonoscopy reaches the terminal ileum at best. Everything in between was essentially invisible territory.
The swallowable camera capsule changed that. And with this technology came the ability to diagnose conditions that previously required invasive surgery or simply went undetected.
So what conditions can capsule endoscopy actually diagnose? The list is substantial , and understanding the diagnostic capabilities helps clinicians determine when this technology offers the best path to answers.
The Small Bowel: Why It Matters
Before examining specific conditions , it helps to understand why small bowel visualization matters clinically. The small intestine handles nutrient absorption , contains significant immune tissue and can harbor pathology that causes systemic symptoms without obvious localization.
Patients with unexplained GI bleeding , chronic anemia , abdominal pain or malabsorption may have small bowel disease that standard endoscopy misses entirely. Understanding what endoscopy involves in its various forms clarifies why capsule technology fills a critical diagnostic gap.
Capsule endoscopy works by capturing thousands of images as the camera travels through the digestive tract. These images reveal mucosal detail throughout the small intestine , enabling diagnosis of conditions that would otherwise require more invasive approaches or remain undetected.
Obscure Gastrointestinal Bleeding
Obscure GI bleeding represents one of the most common indications for capsule endoscopy. This term describes bleeding that persists or recurs after negative upper endoscopy and colonoscopy. The source lies somewhere standard scopes can't reach , usually the small bowel.
What conditions causing obscure bleeding can capsule endoscopy diagnose? Several pathologies account for most cases.
Angiodysplasia (also called arteriovenous malformations or AVMs) appears as small vascular abnormalities in the intestinal wall. These fragile vessels can bleed intermittently , causing chronic anemia or occasional visible bleeding. Capsule endoscopy identifies angiodysplasia as red spots or patches against the normal pink mucosa. According to Cedars-Sinai , vascular lesions represent a leading cause of obscure GI bleeding detected by capsule endoscopy.
Small bowel ulcers from various causes (NSAIDs , Crohn's disease , infections , ischemia) can bleed without causing symptoms that localize to the small intestine. Capsule imaging reveals ulcers as mucosal breaks , erosions or deeper lesions depending on severity.
Small bowel tumors , both benign and malignant , may present with bleeding as their primary symptom. Capsule endoscopy can identify masses , polyps and other growths that standard imaging might miss.
The diagnostic yield for capsule endoscopy in obscure GI bleeding ranges from 40% to 70% depending on patient selection and timing. Performing the study closer to an active bleeding episode improves detection rates.
Crohn's Disease
Crohn's disease can affect any part of the digestive tract , but it frequently involves the small intestine , particularly the ileum. Diagnosing small bowel Crohn's and assessing disease extent represents a major application of capsule endoscopy.
What conditions related to Crohn's can capsule endoscopy diagnose or evaluate?
Initial diagnosis in patients with suspected Crohn's but negative colonoscopy and inconclusive imaging benefits from capsule evaluation. Small bowel Crohn's may exist without ileal involvement visible during colonoscopy. Capsule endoscopy detects mucosal ulcerations , erosions , strictures and the characteristic "cobblestone" appearance of advanced disease.
Disease extent assessment matters for treatment planning. Capsule endoscopy can reveal how much of the small bowel is affected , information that influences medication choices and prognosis.
Postoperative recurrence monitoring in Crohn's patients who've had surgical resection helps detect early recurrence at anastomotic sites or in previously uninvolved segments. Early detection allows treatment adjustment before symptoms develop.
Mucosal healing assessment during treatment helps determine whether current therapy is working at the tissue level , not just controlling symptoms.
One important caveat: capsule endoscopy carries risk in Crohn's patients with known or suspected strictures. The capsule can become lodged in narrowed segments , potentially requiring endoscopic or surgical retrieval. Patency capsules (dissolvable test capsules) or imaging studies often precede capsule endoscopy in Crohn's patients to assess for strictures.
Celiac Disease
Celiac disease primarily affects the small intestine , making capsule endoscopy a logical diagnostic tool. While duodenal biopsies during standard upper endoscopy remain the diagnostic standard , capsule endoscopy plays several roles in celiac evaluation.
Extent of involvement beyond the duodenum becomes visible with capsule imaging. Some celiac patients have damage extending further into the jejunum or even ileum. Understanding disease extent may have prognostic implications.
Complicated celiac disease evaluation helps when patients don't respond to gluten-free diet as expected. Capsule endoscopy can identify ulcerative jejunitis , strictures or other complications. It can also detect small bowel lymphoma , a rare but serious complication of long-standing celiac disease.
Refractory celiac disease workup benefits from capsule visualization to assess mucosal status and look for complications when patients remain symptomatic despite strict dietary adherence.
The National Institute of Diabetes and Digestive and Kidney Diseases notes that while small bowel biopsy remains essential for celiac diagnosis , capsule endoscopy provides valuable information about disease extent and complications that standard endoscopy cannot assess.
Small Bowel Tumors
Small bowel tumors are relatively rare compared to gastric or colorectal malignancies , but they do occur. Capsule endoscopy has improved detection of these often-elusive lesions.
What tumor-related conditions can capsule endoscopy diagnose?
Primary small bowel cancers including adenocarcinoma , carcinoid tumors , lymphoma and gastrointestinal stromal tumors (GISTs) may appear as masses , ulcerated lesions or areas of mucosal irregularity. Many small bowel cancers present with nonspecific symptoms like bleeding , obstruction or pain , making visualization essential for diagnosis.
Metastatic disease to the small bowel from melanoma or other primary cancers can manifest as small bowel lesions detectable by capsule imaging.
Benign tumors including lipomas , adenomas , leiomyomas and hamartomas appear as smooth masses or polyps. While benign , some carry malignant potential or cause symptoms requiring intervention.
Polyposis syndromes with small bowel involvement (Peutz-Jeghers syndrome , familial adenomatous polyposis , juvenile polyposis) benefit from capsule surveillance. These inherited conditions produce polyps throughout the GI tract , and monitoring small bowel polyp burden guides management.
For tumor detection , capsule endoscopy offers advantages over radiologic imaging. Small mucosal lesions that CT or MRI might miss become visible on capsule images. However , capsule endoscopy cannot obtain tissue samples , so identified lesions typically require follow-up with device-assisted enteroscopy for biopsy.
Vascular Abnormalities
Beyond angiodysplasia associated with bleeding , capsule endoscopy diagnoses various vascular conditions affecting the small bowel.
Hereditary hemorrhagic telangiectasia (HHT or Osler-Weber-Rendu syndrome) causes vascular malformations throughout the body , including the GI tract. Capsule endoscopy identifies the extent of small bowel involvement , guiding treatment decisions.
Portal hypertensive enteropathy in patients with liver disease can cause small bowel vascular changes similar to portal hypertensive gastropathy. Capsule imaging reveals the characteristic mucosal patterns.
Blue rubber bleb nevus syndrome produces venous malformations that can bleed significantly. Capsule endoscopy maps small bowel involvement.
Radiation enteritis from abdominal or pelvic radiation therapy damages small bowel mucosa and vasculature. Capsule endoscopy visualizes the extent of radiation-induced changes including telangiectasias , ulcers and strictures.
Inflammatory and Ulcerative Conditions
Several inflammatory conditions affecting the small bowel fall within capsule endoscopy's diagnostic reach.
NSAID enteropathy describes small bowel injury from nonsteroidal anti-inflammatory drugs. Many NSAID users develop small bowel ulcers , erosions or strictures without knowing it. Capsule endoscopy reveals these lesions in patients with unexplained anemia or GI symptoms.
Eosinophilic enteritis produces inflammation with eosinophil infiltration of the small bowel wall. Capsule imaging shows mucosal abnormalities , though definitive diagnosis requires histology.
Behçet's disease can cause intestinal ulcers , particularly in the ileocecal region but sometimes throughout the small bowel. Capsule endoscopy helps assess extent and monitor treatment response.
Intestinal tuberculosis , more common in endemic regions , produces ulcers , strictures and other findings visible on capsule imaging.
Graft-versus-host disease affecting the gut in bone marrow transplant recipients can involve the small intestine extensively. Capsule endoscopy helps assess disease severity and extent.
Malabsorption Syndromes
When patients present with malabsorption symptoms (diarrhea , weight loss , nutritional deficiencies) and standard testing is inconclusive , capsule endoscopy can identify small bowel pathology responsible for impaired absorption.
Lymphangiectasia appears as dilated lacteals visible on capsule imaging. This condition causes protein-losing enteropathy and fat malabsorption.
Whipple's disease , a rare bacterial infection , produces characteristic pale , shaggy mucosa in the small intestine.
Small intestinal bacterial overgrowth (SIBO) itself isn't directly diagnosed by capsule endoscopy , but structural abnormalities predisposing to SIBO (strictures , diverticula , surgical blind loops) become visible.
Autoimmune enteropathy produces villous atrophy similar to celiac disease but without gluten sensitivity. Capsule imaging helps assess extent while biopsies confirm the diagnosis.
What Capsule Endoscopy Cannot Diagnose
Understanding limitations is as important as knowing capabilities. Capsule endoscopy has real constraints.
Submucosal lesions may be missed if they don't produce visible mucosal changes. Some GISTs and other tumors grow beneath the surface without obvious luminal abnormality.
Motility disorders aren't diagnosed by capsule imaging , though abnormal transit times might suggest dysmotility.
Functional conditions like irritable bowel syndrome have no visible mucosal findings and won't show abnormalities on capsule endoscopy.
Definitive histologic diagnosis requires tissue. Capsule endoscopy identifies lesions but cannot sample them. Suspicious findings need follow-up with enteroscopy or surgery for tissue confirmation.
Gastric and colonic pathology may be captured incidentally , but capsule endoscopy isn't optimized for these regions. Standard endoscopy remains superior for stomach and colon evaluation.
Clinical Decision Making
When should clinicians order capsule endoscopy for diagnosis? The strongest indications include obscure GI bleeding after negative bidirectional endoscopy , suspected small bowel Crohn's disease , evaluation of known Crohn's extent , suspected small bowel tumors , surveillance in polyposis syndromes and assessment of celiac disease complications.
The technology works best when there's reasonable suspicion of small bowel pathology based on symptoms , laboratory findings or imaging. Using capsule endoscopy as a screening tool in low-probability situations reduces diagnostic yield and may not represent optimal resource utilization.
Capsule endoscopy has expanded diagnostic capability significantly. Conditions that once required surgical exploration or simply went undiagnosed now have a noninvasive path to visualization and identification. For small bowel pathology , the swallowable camera has become an indispensable diagnostic tool.
© 2025. All rights reserved.
About Us
Introduction
Development
Cooperation
Service
Main Products
Medical Grade Monitor
No 15, Jinyang road KunshanSuzhou, Jiangsu, China
